Kent E. Dicks, Founder & CEO of Life365, shares his perspective on how telemedicine and virtual care can help address the VA’s growing physician shortage and expand access for veterans.
How to Economically Scale Remote Patient Monitoring to Larger Populations
Remote Patient Monitoring (RPM) is not a new concept, it has been around for many decades, in various different forms. The main purpose of RPM, is to connect patients outside of the hospital setting, typically at home, to a central location for monitoring, in order to help prevent visits to the ER and hospitalizations which reduces healthcare costs. This is accomplished by capturing vital signs, and other indicators of well-being, and transmitting the data to care providers for notification and review.
During the COVID-19 pandemic, Telehealth (a video visit with a doctor) adoption exploded overnight, going from about 10-12% utilization to nearly 70%, as of March 2020. For many, it was the only option available for individuals to see their doctors due to offices closing face to face visits in fear of spreading COVID. One would think that Remote Patient Monitoring would have seen similar growth during the same timeframe, with the benefits of monitoring people remotely like, keeping critical healthcare resources safe or saving clinical trials that were under threat to be stopped due to the inability to have face to face visits, but due to many factors, RPM adoption did not increase significantly in 2020 / 2021.
One of the reasons for lack of RPM adoption was healthcare resources were still challenged with adopting Telehealth visits, and needed to drastically change their clinical workflow (how they interacted with patients). Other variables included billing requirements that left financial risk for providers seeking to monitor patients remotely; they had to ensure the patient took at least 16 days of readings in a 30 day period to receive reimbursement, and patient engagement/ compliance can be a daunting task to manage. Health systems were struggling financially during the pandemic because they could not do elective procedures, where they make a bulk of their revenue. Ultimately, introducing a new service, that doesn’t pay as much as face to face visits, or using it for COVID patients, which has a short term monitoring period (for most), made it not cost effective to deploy the technology.
Scaling to a Greater Population of Patients
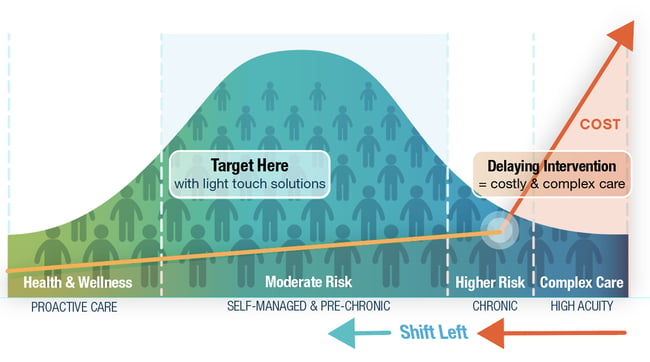
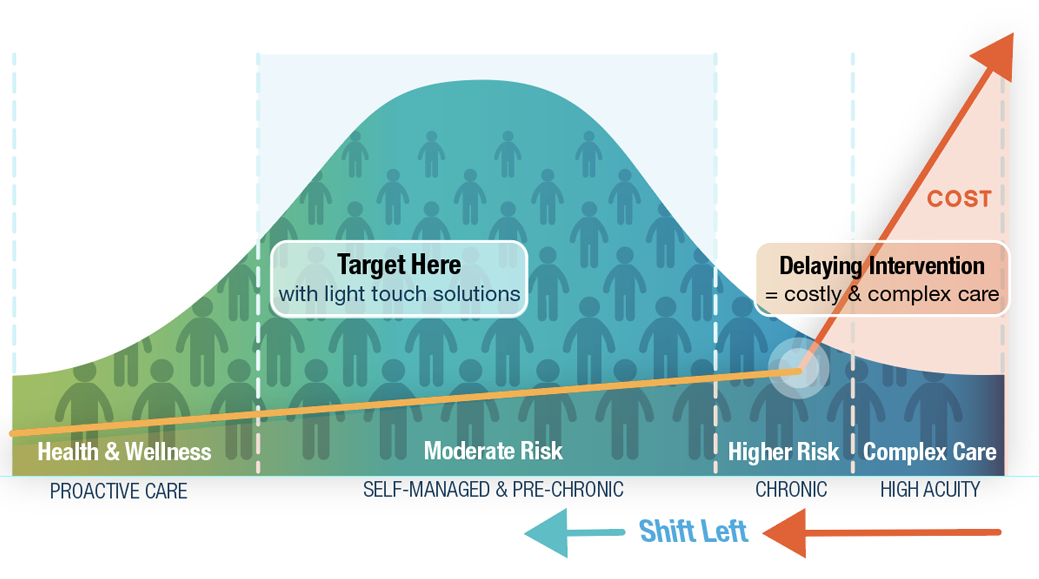
We have created a graph called “The Hump”, which shows how patients are clustered on the continuum of care. On the left hand side are health and wellness individuals – a sizable number of individuals, with very little impact on quality of care and costs. On the right hand side is complex care – This is 5% of the population that consumes 50% of healthcare costs. A large amount of money is being spent in complex care, so deploying Remote Patient monitoring, with its barriers to adoption, “friction points”, makes sense, financially. The problem with using remote monitoring with complex care, is that you typically have to wait until the person is sick enough/costly enough before you are justified to deploy the RPM solution, thus producing a reactive strategy.
In the middle of the hump, are individuals that are becoming, or are newly chronic, whom are not costing a lot of money, just yet. This is a much larger population of people that healthcare entities are at risk for, and have the opportunity to be proactive, stopping their progression to a more costly state. For this group, traditional RPM would not be cost effective and it requires different ways to engage these individuals in their care. In order to reach greater populations of individuals, we need to remove the “Friction Points” that impede scaling.
Removing the Friction Points to Scale
Remote Patient Monitoring has traditionally been hard to scale because of “Friction Points” involved in the process. Because of these friction points, RPM is oftentimes only deployed with the sickest of the sick, complex care, where the amount of money being spent in healthcare dollars justifies the expense and effort to deploy the needed connected technology to the patient. These friction points (or barriers to scaling) include:
- Cost of Equipment
- Lack of initiation from within the EHR
- Alignment of the appropriate connected solutions
- Logistics and distribution
- Lack of data in a single clinical repository
- Patient engagement
- Payment / Reimbursement
Cost of Equipment
In the beginning, Remote Patient Monitoring was very expensive to deploy, with large remote cameras, like those found in TV stations, hooked to monitors, transmitting back to a remote location for a physician to review, diagnose and recommend therapy. It later transitioned to a central “hub” device that may be faceless, connected via a plain old telephone system (POTS) line to wired medical devices: Scales, Blood Pressure, Pulse Oximeter, Glucometers and more. These systems were expensive, $4,000-$5,000 each, which meant they were only feasible to deploy with patients that were very sick, consuming large amounts of healthcare dollars, and frequenting the hospital.
High costs required that the equipment be returned when a patient was finished, then refurbished, recalibrated, and re-distributed to another patient for use. Today, we have wireless Bluetooth medical devices, and the cost of that equipment has plummeted drastically, with total costs as low as $100 for devices and connectivity. This means we can afford to deploy RPM solutions with a greater population of patients, and that refurbishment, recalibration, and redistribution are no longer a requirement due to cost of equipment. Cost of equipment is a diminishing contributing factor to the barrier of scaling.
A benefit of moving from wired to wireless (Bluetooth / cellular) medical devices is the fact that the equipment can be deployed throughout a home, instead of having to go back to a wired location connected to the hub to take their readings. Studies have shown that adoption of home remote patient monitoring increases when devices are in their natural location – scale in the bathroom, glucometer in the kitchen, blood pressure by the chair in the den, and pulse oximeter on the night stand in the bedroom.
Lack of Initiation from Within the EHR
Another friction point is the prescribing or initiation of a remote patient monitoring solution for a patient. Physicians are extremely busy in their day to day routine within their practice. Trying to figure out how to connect a patient to a remote patient monitoring solution can be a major barrier to scaling. Clinicians commonly work within a single Electronic Health Record (EHR) for patient records and treatment. The more that the prescription of the RPM solution can be done within that same EHR increases, the chance of utilization and adoption of RPM technology by clinicians. Once an order is initiated by the clinician from within the EHR, it is forwarded to the integrated digital health platform for selection, shipping, engagement and integration of the patient’s data for the clinician to review in the same EHR. The clinician simply initiated an order and waited for the data to come back in from the patient in the coming days to begin remote monitoring and the ability to bill for remote services.
Alignment of the Right Connected Solutions
Many times, a clinician will complete a care plan for a patient that asks them to take vitals for their specific condition. This care plan may ask the patient to take their blood pressure twice a day, their weight once a day in the morning, their pulse oximeter reading (SPO2) twice a day and their Glucose levels four times a day. The clinician didn’t specify what devices were to be used, or how they would be connected to the clinical backend and the patient's record. Requiring a clinician to know what brands and configurations of devices to order to capture the requested vitals is a heavy lift and impedes scaling the solutions to home. We want clinicians to be clinicians, not technicians.
The digital health platform should ingest the care plan and make the decision on what kit / configuration is appropriate to deploy for a specific demographic of patients. There is opportunity in this area to use machine learning / AI to gather insights as data flows through the platform to understand how certain cohorts adopt certain technology configurations and make recommendations on what to kit and configure based not only on the care plan, but also the demographics of the individual patient. We call this solution the Personalyze™ system, which is an ever-learning system to not only align the right solution, with the right patient, to get the right outcome, at the right cost, but also to help engage the patient in the use of that solution to maximize adherence.
Logistics and Distribution
Another large barrier to scaling, is a clinician having to figure out how to deploy a selected kit / configuration to a patient at their home. We have seen many models to help with accomplishing this task, including kits being preconfigured and sent to the clinician’s office to hand to the patient at the point of care, and providing an initial training. Under new RPM CPT codes, the clinician would qualify to receive reimbursement for the training of the patient on the system. Another method is to have the order entered into the EHR, then sent to the digital health platform where the kit / configuration is selected, which then sends an order to the logistics vendor to ship out the kit to the patient’s home. It arrives pre-configured, with clear / simple instructions for use. A third option is sending pre-configured kits to a third party partner that provides care at home to a patient (Home Healthcare, Nurse Navigators, Fast Response Teams, etc.) to stabilize the patient, connect them with the equipment, and monitor the patient via a nurse call center. There are multiple models that are emerging where paramedics are acting as Nurse Navigators (Dispatch Health, AMR Ambulance, etc.) creating “Fast Response Teams” to stabilize the patient at home, connect to a nurse call center for monitoring, instead of transporting them to the ER / hospital which is much more expensive. In the future, connected solutions providing data to cloud based machine learning / analytics will be able to produce “Just in Time Care,” determining when to visit a patient based on trends from data received in near real-time.
Lack of Data in Single Clinical Repository
Clinician adoption is increased dramatically by having all patient data in a single repository / EHR. Changes to their clinical workflow impede the adoption of new technology and solutions, and lead to resistance in implementing a RPM solution with their patients. By being able to initiate the RPM request from within the EHR, and have the data displayed back in that same EHR, it increases the likelihood that a clinician can seamlessly adopt RPM technology across a broader population of their patient base. It would be important to include patient identification, onboarding, activity time tracking, documentation, and billing.
Patient Engagement
One of the requirements of the RPM CPT codes is that a patient must take 16 days of biometric readings, within a 30 day time period, from a wireless connected medical device to qualify for reimbursement. The clinician does not have the time to engage each and every remote patient in taking their readings, and they certainly do not want to pay for RPM solutions each month, if they are not able to bill for that individual patient. RPM solutions must provide services to engage the clinicians' patients to ensure they take their readings, and provide alerts / notifications in advance to the clinical team if they are in danger of not receiving the 16 days of readings and are left unable to bill.
Payment / Reimbursement
For the longest time, the use of remote patient monitoring was only beneficial to healthcare entities that were financially responsible for a group of patients, in order to keep them out of the ER / hospital to reduce costs, improve their quality of care, and profitability (impacting reimbursement through STAR and HEDIS ratings).
Today, the physician practices are able to bill for Chronic Care Management (CCM), Remote Patient Monitoring (RPM) and as of January 1, 2022, Remote Therapeutic Monitoring (RTM) which deals more with compliance / adherence, such as medication and therapy compliance, and more.
Now that reimbursement is in place, clinicians are more inclined to adopt remote care, along with telehealth to offer a virtual care bundled solution. In fact, since the pandemic and the spike in Telehealth adoption virtually overnight, clinicians have seen the immense benefit in virtual care and have changed their clinical workflow to be more inclusive of virtual care, and less about face to face and brick and mortar office visits. Many practices are adopting a “Hybrid” approach, especially specialty care, to see a patient at least once a year in the office, and provide other visits virtually.
The Evolution of Remote Patient Monitoring
As stated before, remote patient monitoring has been around for many decades in many shapes and forms. What is important to note from “The Hump” that we have developed, is that RPM has traditionally concentrated on the right hand side of the chart, “Complex Care” with a small patient population and a larger technology footprint. What is needed is a “Shift Left” into the middle of the hump to increase the impact to larger populations, with little to no initial technology footprint, in order to make the economics work. Below are the areas of RPM through the ages. Today we are currently implementing RPM 2.0, but need to quickly move to RPM 3.0 and 4.0 to maximize the cost savings and engagement in a larger population.
RPM 1.0
As mentioned previously, remote patient monitoring started with TV cameras hooked up in remote locations to wired “Hubs” connected to Plain Old Telephone Systems (POTS) lines to wired devices (Scale, Blood Pressure, Pulse Oximeters, Glucometers and more), sending the data into a central location for clinicians to review remotely. The cost of these systems could be up to $4000-$5000 and often required a technician to install, which increased the cost even more. Because of the cost of the solution, it was often used with the sickest of the sick and was retrieved at the end to be cleaned, refurbished, recalibrated and distributed to a new patient. This impeded scalability to a broader population of patients proactively. It was used more reactively once a patient started to consume more healthcare resources in an effort to stop ER visits and ultimate hospitalizations.
RPM 2.0
This is the next generation of technology that used wireless (Bluetooth) devices (scale, blood pressure, pulse oximeter, glucometers, spirometers, EKG and more) connected through cellular devices (Smart Phone, Tablets, IoT Hubs or Cellular Embedded Devices) to send data to the cloud and into the clinical backend for review by Machine Learning / AI or Analytic systems and/or a clinician. As mentioned before, many of these kits / configurations use equipment that costs $100 or less (not including the Smart Phone, Tablet or Hub) which means it's not cost effective to retrieve the equipment for refurbishment and redistribution. It's often better to ship a kit to a patient, leave it with them for off and on use over time. This definitely allowed more patients to be monitored, because of ease of deployment and cost, than RPM 1.0. Today, this market in the US is only about $150M in revenue and the number of competitors in this space is growing by the day. The upside is that new consolidated Telehealth platforms with payers, becoming “Payviders,” will need to own their own RPM platform, not sharing with their competition. Providers will need to connect outside their communities to access patients that the Telehealth platforms have taken away, so they will be acquiring RPM solutions for themselves as well (at least the large health systems will own their own virtual care platform).
Moving to Greater Populations – Preemptive Care
New models of care have emerged, which need to receive near real-time data from a patient to identify who might be de-comping at home, and potentially heading to the ER and being hospitalized.
Actionable data is the key to connecting to a remote population of patients. Machine Learning / AI Analytic systems are thirsty for a large amount of data to monitor a large population of patient to see outliers that need attention to head them off from going to ER and ultimately being hospitalized, increasing healthcare costs.
Technology is evolving at a rapid pace that can help acquire this cost-effective actionable data from the patient at home. Two tiers of actionable data, which are now coming into play because of advancement of technology, include RPM 3.0 and 4.0, which can be identified on “The Hump.”
RPM 3.0
As we start shifting “Left” away from expensive Complex Care and into the middle of the hump, we start using less of a technology footprint and more lightweight, disposable technology that is disposable or non-visible (“Disappearables”) around the body, creating a body area network of devices and solutions connected to the cloud with light weight sensors. New cost-effective, disposable grade technology has been developed in flexible circuitry / batteries, lean operating systems, utilizing ultra wide area and narrow band IoT Networks, sending small amounts of data across long distances consuming less power and having long battery life. This makes the devices super cost-effective, and usable by seniors and large populations of individuals. This class of connected solutions (wearables, sensors and patches) communicates with OEM medical devices, rapid diagnostics, implantable devices and home connected devices like Smart TV / remotes, security systems and more. The biggest opportunity with this technology platform is to drive the devices through Machine Learning / AI and to use exception based processing to “Nudge” an individual into compliance, comparing them to their own data using “Lite” cost-effective sensor data as a first tier approach. This approach allows a greater population to be addressed, and to help drive that greater population into compliance as an Intelligent Digital Therapeutic (iDTx), leaving a smaller population to address as a Tier 2 with more expensive solutions, such as RPM 2.0. Companies like Life365 / LifeConnect have been very fortunate to have been issued US Patents on this next generation of RPM technology, and are working with partners to license and implement to help scale across large populations of patients.
RPM 4.0
This is targeted smack in the middle of the hump and is truly the first line of connected solution using no deployed technology other than a Smartphone, Tablet, Computer or TV to send biometric and behavioral feedback to the cloud. With the advent of facial augmentation and the improvement of consumer grade cameras, the ability has arisen to gather key vital sign data using consumer grade equipment that is most likely in a consumer's possession. Telehealth and remote behavioral health has clearly ramped up in adoption over the last several years. Most Telehealth visits are still episodic in nature, and need to shift to chronic care management. With the management of chronic conditions remotely, this technology allows the clinicians to gather at least some base lines to make an initial evaluation without having to deploy technology remotely. We believe that facial augmentation will play a key role in starting the connected health journey with a large population of patients remotely, then gradually move right choosing the appropriate level of connected solutions needed to help take care of the patient remotely.
Coming Up in the Next Chapter
Going forward into 2022 and beyond will be a year about consolidation, “Bundling” and personalizing solutions specifically for an individual to maximize adherence. This personalization will take into account the “Whole Person Solution” to truly understand what engages people, and provide the tools in their care to maximize the outcomes (Telehealth, RPM, Behavioral Health, Transportation, Med Compliance, Food, Social Determinants of Health and much more).
Latest Resources
Stay informed with our latest news, resources, and insights!
-1.png)

-1.png)
-1.png)