Kent E. Dicks, Founder & CEO of Life365, shares his perspective on how telemedicine and virtual care can help address the VA’s growing physician shortage and expand access for veterans.
The Centers for Medicare and Medicaid Services (CMS) released the 2022 Medicare Physician Fee Schedule (MPFS) proposed rule July 23rd 2021. Within the rule, five new CPT® codes were proposed for Remote Therapeutic Monitoring (RTM). We discuss the codes, their implications, and issues that still remain to be addressed in the final rule below.
What are the Five New Remote Therapeutic Monitoring (RTM) Codes?
The codes provide exciting new opportunities to expand virtual care, with the ability to capture non physiologic health data from patients, as well as an expansion of eligible practitioners that can offer services, particularly, the types of practitioners who were ineligible to offer Remote Physiologic Monitoring (RPM) services.
The new RTM codes closely resemble the existing Remote Physiologic Monitoring (RPM) codes. The codes include three technical component codes with no professional work required, and two professional component codes.
As outlined in the MPFS proposed rule, the codes are as follows;
- CPT® code 989X1 - Remote therapeutic monitoring (e.g., respiratory system status, musculoskeletal system status, therapy adherence, therapy response); initial set-up and patient education on use of equipment
- CPT® code 989X2 - Remote therapeutic monitoring (e.g., respiratory system status, musculoskeletal system status, therapy adherence, therapy response); device(s) supply with scheduled (e.g., daily) recording(s) and/or programmed alert(s) transmission to monitor respiratory system, each 30 days
- CPT® code 989X3 - Remote therapeutic monitoring (e.g., respiratory system status, musculoskeletal system status, therapy adherence, therapy response); device(s) supply with scheduled (e.g., daily) recording(s) and/or programmed alert(s) transmission to monitor musculoskeletal system, each 30 days
- CPT® code 989X4 - Remote therapeutic monitoring, physician/other qualified health care professional time in a calendar month requiring at least one interactive communication with the patient/caregiver during the calendar month; first 20 minutes
- CPT® code 989X5 - Remote therapeutic monitoring treatment management services, physician/other qualified health care professional time in a calendar month requiring at least one interactive communication with the patient/caregiver during the calendar month; each additional 20 minutes (List separately in addition to code for primary procedure)
Primary Differences Between RPM and RTM Codes
While the new remote therapeutic monitoring (RTM) codes were structured to resemble the remote physiologic monitoring codes, CMS outlines in the proposed rule two primary differences.
- New range of practitioners who can furnish services
The new RTM codes were designed to enable practitioners that are unable to furnish services and bill the remote physiologic monitoring (RPM) codes, to furnish and bill for services that look similar to RPM. CMS specifically mentions nurses and physical therapists as projected to be the primary billers of these codes.
Physical therapists are unable to bill evaluation and management codes (E/M codes), and were therefore unable to utilize the RPM codes which were considered E/M services. Therefore, the new RTM codes are instead general medicine codes with the intent of enabling other practitioners to furnish services that are similar in nature to RPM. - New types of data that can be captured and evaluated and how it can be collected
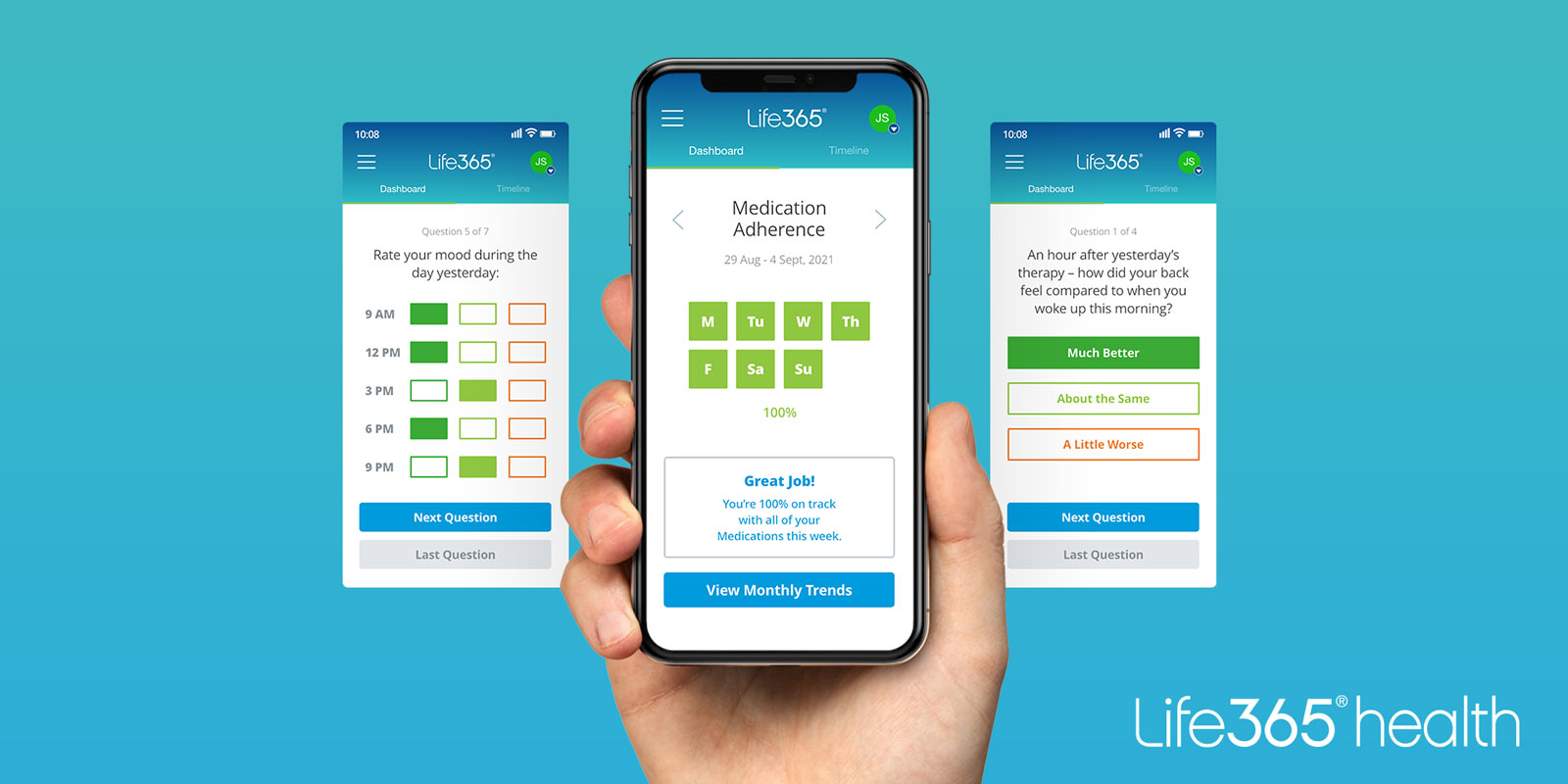
While the RPM codes capture physiologic data, the RTM codes allow non-physiologic data to be collected, like medication adherence and pain levels. RTM data can be self-reported as well as digitally uploaded. The RPM codes require data to be physiologic and the data must be automatically captured and digitally uploaded/ transmitted by a connected device.
Other Takeaways / Issues to be Addressed
- Limited use cases
Unlike RPM, which can be offered to patients with one or more acute or chronic conditions, RTM services are limited to the monitoring of musculoskeletal and respiratory conditions. As they are written now, CPT® Code 989X2 is for a device monitoring respiratory system status, and CPT® Code 989X3 is for a device monitoring musculoskeletal system status. This is not only limiting in the types of conditions that can be monitored, but also the types of devices, software, and applications that can be used to capture other important information like medication adherence, mood, pain, symptoms, etc. - Who, exactly, can bill for RTM?
The proposed rule mentions physical therapists and nurses as suspected “primary billers,” but do other therapists, such as occupational and speech therapists qualify? Do other qualified healthcare professionals, such as psychologists qualify to bill for these services? - Can RTM be provided “incident to” a physician, nurse practitioner, or physician assistant?
CMS designated RPM codes 99457 and 99458 as “care management services” which allows physicians and QHPs to bill 99457/99458 under “incident to” service rules, meaning clinical staff or auxiliary personnel may perform services associated to 99457/99458 under the general supervision of the billing physician or QHP. RTM are not E/M codes, and therefore cannot be designated as care management services, thereby not allowing “incident to” service rules. This is contrary to what CMS mentioned in the proposed rule, as they stated they suspected nurses to be primary billers. Unlike the RPM codes, there is no mention of “clinical staff” in the code descriptors.
Because the RTM codes are not E/M codes, they cannot be designated as “care management” services which allows services to be rendered “incident to” a billing provider. This excludes physical therapists and other practitioners that are not physicians or NPPs to bill the RTM codes - which is the opposite of CMS’s intent. As a result, CMS is seeking comment on how best to “remedy the issues related to the RTM code construction in order to permit practitioners who are not physicians or NPPs to bill the RTM codes.”
Conclusion
The new RTM codes help expand virtual care services, enabling practitioners and patients to use digital technologies that improve patient care, and the patient experience. While the new codes are a great step forward, there are still quite a few questions that need to be answered, and details that need to be resolved for the final rule. CMS acknowledges this, and is requesting feedback.
Call to Action
Stakeholders interested in RTM should consider providing comments to the proposed rule. CMS is accepting comments on the proposed rule until September 13, 2021. You can submit your comments as an individual, an organization, as well as anonymously at the link, here.
To access the 2022 Medicare Physician Fee Schedule proposed rule, click here.
To stay current with the latest developments regarding remote patient monitoring and remote therapeutic monitoring, subscribe to our blog and follow Life365 on social media.
Latest Resources
Stay informed with our latest news, resources, and insights!
-1.png)

-1.png)
-1.png)