Kent E. Dicks, Founder & CEO of Life365, shares his perspective on how telemedicine and virtual care can help address the VA’s growing physician shortage and expand access for veterans.
RPM, combined with PERS, improves quality of life and health outcomes for older adults
- Blog
- |
- January 25, 2022
According to the CDC, approximately 85% of older adults have one or more chronic conditions, and 60% have two. Older adults living with chronic conditions may be living with the loss of independence, physical function, and well-being. Older adults also face an increased risk for falling. One in four older adults fall each year, and falling once doubles your chance for falling again. Falls are very costly, with more than 800,000 individuals being hospitalized for head injuries or hip fractures.
With challenges older adults living with chronic conditions face, remote patient monitoring and personal emergency response solutions combined together can lead to longer independence and better health outcomes. We discuss the benefits of both, and why RPM and PERS, together, can help older adults lead healthier lives and remain independent longer.
Remote Patient Monitoring (RPM)
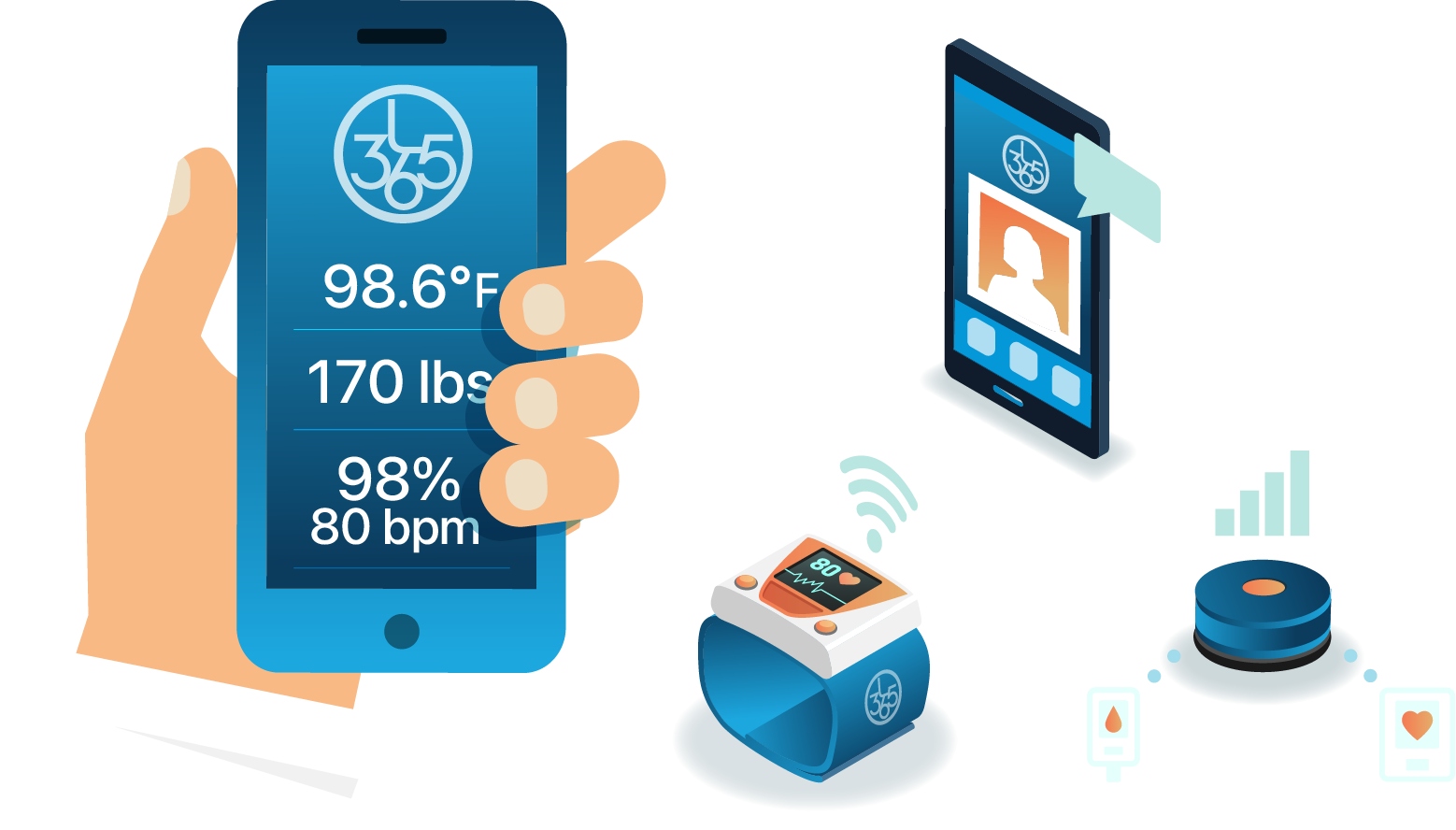
Remote patient monitoring uses technologies to capture and collect health data from individuals, and transmit that data to healthcare providers in another location for review. Data captured often includes vital signs like weight, blood pressure, blood oxygen levels, glucose levels, as well as other data like medication compliance or symptoms.
For high-risk patients and complex care patients, RPM can help prevent avoidable hospital admissions and readmissions, and enables providers to point patients to appropriate levels of care, if needed.
For patients with chronic conditions, RPM enables patients to monitor and manage their conditions, and provides care team members, health coaches, and family members with data insights for more informed care decisions and disease management education.
RPM transforms healthcare delivery from a reactive care model to a proactive care model, which can lead to reduced costs of care, and a better quality of life for patients.
Fueled by new remote patient monitoring reimbursement codes, RPM is more accessible for older adults than ever before. It is financially feasible for providers and health systems to invest in remote patient monitoring programs for their patients. For many older adults, this means a low cost or no out of pocket cost virtual care management program through Medicare.
Personal Emergency Response Services (PERS)
PERS devices can be used to collect information about an older adult's status and summon help should there be an emergency. They are often used as a fall alert system for older adults. PERS can come in various forms, including wearable pendants, sensors, stationary hubs. They can be used to capture movement around a home, monitor an individual's location, specific activities, falls, and more. The information is captured and transmitted to another location, such as an emergency call center or family member.
According to the CDC, more than one out of four older people falls each year, but less than half tell their doctor. In 2015, medical costs for falls totaled more than $50 billion, and Medicare and Medicaid shouldered 75% of these costs. If a fall occurs, and assistance is provided in less than 3 hours, there is an 88.5% chance your loved one will return home. Longer than 12 hours, and the chance for returning home drops to 2.7%. Falls and fall-related injuries are highly prevalent but preventable, and health care providers play a crucial role in helping older adults reduce their risk for falls.
Helping older adults lead healthier lives by managing their chronic conditions, can lead to greater physical function that reduces fall risk factors, demonstrating the importance of integrating RPM and digital health tools into a care management program.
Care Transitions
New models of care are emerging, with a focus on shifting more care to the home, where patients are most comfortable. The Hospital@Home program provides hospital-level care in a patient's home as a full substitute for acute hospital care.
For patients transitioning home from an acute care stay, especially if they may be spending time alone at their home after transitioning home, having RPM and PERS provides the patient with additional support during this critical time period.
RPM enables care teams and family members to continue to monitor vitals and medication adherence, and intervene should they detect a deterioration in health status. PERS ensures patients have easy access to connect with a call center at the push of a button should they need help. These tools could enable patients to recover at home, instead of a higher level of care like a skilled nursing facility. This would reduce costs, and provide a better patient experience.
Conclusion
RPM + PERS get patients involved in their own care. They are more likely to be compliant as they understand they are being monitored. Remote patient monitoring and PERS benefits patients by providing them with easy to use tools to manage their conditions, and help them stay connected to their care team and loved ones to help ensure better health outcomes and longer independence.
Who could benefit from PERS and Remote Patient Monitoring?
- Adults living with chronic conditions and reduced physical mobility
- Older adults spending most or part of their days alone
- Individuals that have been recently hospitalized due to chronic or acute conditions
- Individuals that could benefit from medication management and monitoring
- Those that need an expanded team of support to help manage their health and care coordination
Latest Resources
Stay informed with our latest news, resources, and insights!
-1.png)

-1.png)
-1.png)