Kent E. Dicks, Founder & CEO of Life365, shares his perspective on how telemedicine and virtual care can help address the VA’s growing physician shortage and expand access for veterans.
RPM has helped many healthcare organizations reduce readmissions, decrease cost of care, and improve patient outcomes. While we've highlighted some key use cases for remote patient monitoring, with more providers leveraging digital health tools, use cases will continue to grow.
Hospital at Home
What is Hospital at Home? According to CMS, “The Acute Hospital Care at Home program is an expansion of the CMS Hospital Without Walls initiative launched in March 2020 as a part of a comprehensive effort to increase hospital capacity, maximize resources, and combat COVID-19 to keep Americans safe. This program creates additional flexibility that allows for certain health care services to be provided outside of a traditional hospital setting and within a patient’s home.”
For a hospital to apply to participate in the program, there are several requirements that must be met. Today, there are more than 100 hospitals participating in the program, helping patients receive care and recover in the comfort of their home. Some notable benefits of a hospital at home program include; an increase in hospital beds, diverting individuals from the ED, decreasing length of stay, reduced costs, better outcomes, and more.
RPM and two-way video telehealth allows caregivers to monitor patient vitals in real time, perform video telehealth consultations, schedule medication reminders, assess symptoms, and provide engaging educational content.
In the future, more care will be moved to the home. It is a win for patients, the healthcare system / hospital, and those financially responsible for the patient’s care (payer).
Home Healthcare
Remote patient monitoring and two-way video provide extra support to the patient in between in person nursing visits, as well as connectivity to their home healthcare team should they have questions or need assistance. Data can be shared with the patient’s provider for health status updates, enabling data driven decision making with faster interventions and therapy adjustments. This could lead to reduced re-hospitalizations, and better outcomes for the patients.
While home healthcare providers cannot bill directly for remote patient monitoring, they can include the costs of remote patient monitoring on the annual cost report forms.
RPM has the ability to augment care provided by the home health agency care team.
Heart Failure Patients
Congestive heart failure is a prominent use case in remote patient monitoring. One of the reasons why, is because of the high rate of readmissions, with nearly 25% of heart failure patients readmitted within 30 days of being discharged.
Hospitals have been keen to curb their readmissions since payment policies (the Hospital Readmissions Reduction Program) were implemented that reduce payments to hospitals with higher readmission rates for heart failure, and a few other conditions.
Some techniques for helping prevent readmissions include;
- Helping improve patient education
- Enabling patient / care team communication
- Medication adherence
- Virtual care monitoring
Remote patient monitoring and telehealth can help deliver critical patient education, post discharge information, and follow up instructions. Medication and appointment reminders help ensure medication regimes are followed appropriately, and the monitoring of vitals can help care team members identify decompensation for faster interventions to help avoid costly, avoidable readmissions.
Primary Care
New remote patient monitoring reimbursement codes have finally made it possible for providers to offer digital health tools and treatment management services between in person visits to patients with chronic or acute conditions. It makes sense for primary care to offer RPM services, as they are often the first point of contact and foundation of a patient’s healthcare team.
Patients struggling to manage their existing chronic conditions, or those who are newly diagnosed, can both benefit from on-going care management and the use of helpful RPM tools to better manage their health and understand their conditions.
Providers have access to a patient’s measurement readings and can better understand the patient’s trends between visits, and response to therapy regimes. This changes the dynamic from reactive care, to preventative care.
The remote physiologic monitoring CPT® codes provide reimbursement for patient training, equipment and data transmission, staff monitoring of measurements, patient education, and other treatment management services that could benefit the patient.
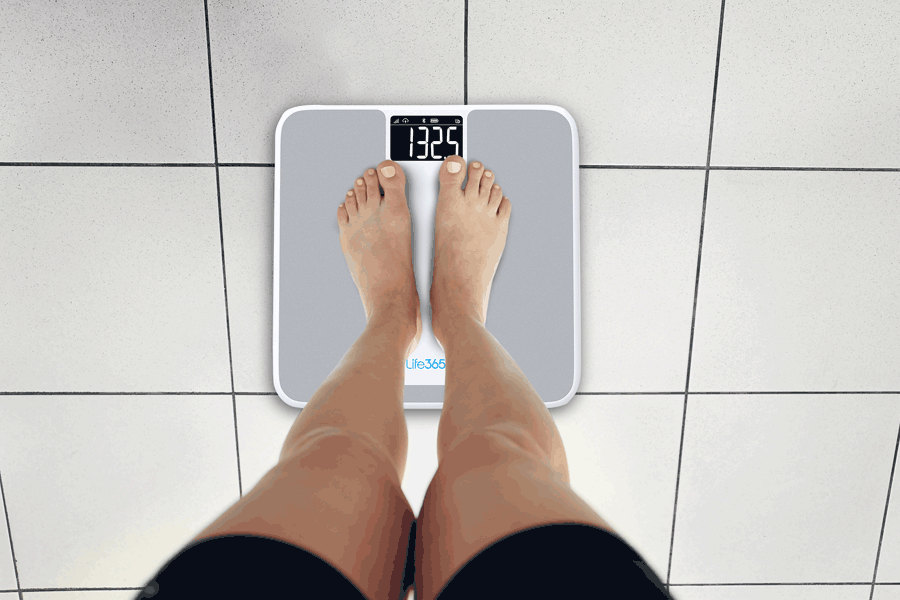
Programs focusing on blood pressure management, diabetes, gestational diabetes, COPD, obesity, and more are all viable options for a remote monitoring program.
Latest Resources
Stay informed with our latest news, resources, and insights!
-1.png)

-1.png)
-1.png)